3 June, 2019
What happens to pancreatic function after surgery?
One of the issues that often generates a great deal of confusion between patients and doctors is changes in pancreatic function following surgery and how to treat it. The worsening of the different pancreatic functions is a well-studied phenomenon, which does not occur in all patients. However, its diagnosis can help to ensure a postoperative period with fewer complications, thereby contributing decisively to a better quality of life for patients.
FUNCTIONS OF THE PANCREAS
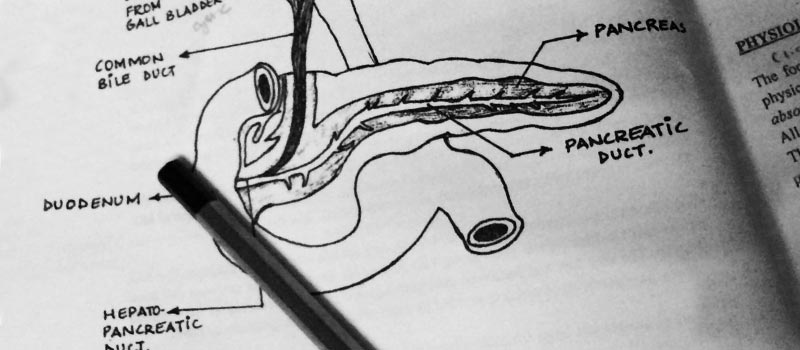
As we have explained in previous blog posts, the pancreas performs two basic functions: it is involved in digestion, secreting substances (pancreatic enzymes) that help in the digestion process and facilitate the absorption of nutrients in the intestine; and it also releases hormones to control blood sugar levels. Respectively, these two functions form part of the so-called exocrine and endocrine functions of the pancreas.
You might be interested in…
– ¿Qué es el páncreas, qué función tiene y cómo enferma?
LOSS OF PANCREATIC FUNCTION OWING TO SURGERY
The amount of healthy pancreatic tissue will decrease to varying degrees depending on the extent and location of the pancreatic surgery. This may lead to a loss of function, which may or may not have a clinical effect. The exocrine and endocrine functions of the pancreas are located in all regions of the pancreas; however, the exocrine function is found primarily in the head of the pancreas, while the endocrine function is more prominent in the body and tail of the organ. In cases of pancreatic tissue-sparing surgery (enucleations, central pancreatectomy or uncinectomy), the amount of pancreatic tissue removed is minimal. As such, a minimal decrease in pancreatic function is expected. In contrast, pancreatic head or body-tail resections may result in a marked deterioration of the exocrine and endocrine functions, respectively. In the most extreme cases of total pancreatectomy there is a total loss of function.
You might be interested in…
– ¿Cuáles son las consecuencias tras la extirpación parcial o total del páncreas? La insuficiencia pancreática
PANCREATIC ENZYME REPLACEMENT THERAPY
The most important aspect is when to treat patients. From the perspective of assessing pancreatic function, a distinction needs to be made: the endocrine function is easily verifiable, and it is highly recommended that patients be assessed before and after surgery by an endocrinology specialist. The endocrinologist will decide on the appropriate treatment based on blood sugar levels. In this regard, the greater the extent of surgical removal, the more pronounced the need for replacement therapy with oral anti-diabetic drugs or insulin will be. On the other hand, assessing a patient’s exocrine function is difficult and often requires invasive tests to obtain reliable results. In this regard, the doctor will need to evaluate the presence, or lack thereof, of clinical abnormalities directly related to malnutrition: weight loss, excessive flatulence due to bacterial overgrowth, steatorrhoea (excretion of fat with faeces) and lab test abnormalities indicating malnutrition. If there are any abnormalities of this type following pancreatic surgery, pancreatic enzyme replacement therapy must be established at sufficient doses, including the combination of drugs to inhibit the secretion of acid by the stomach, in order to reduce enzyme degradation. It is also important to stress that the patient must start replacement therapy when starting the diet in all cases in which the surgery has resulted in the loss of the pancreatic head. High doses will need to administered to reduce the loss of exocrine function. This will help to ensure that the patient has optimal nutrition levels in the postoperative period.
You might be interested in…
– ¿Qué calidad de vida tendré tras la cirugía del páncreas?
– Recuperación de una cirugía del páncreas: Medidas generales a tener en cuenta
– Alimentación en cáncer de páncreas y tras cirugía pancreática



