Colon and rectal cancer is one of the most common neoplasms in Western countries with an incidence of 20-34 cases per 100,000 inhabitants. In Spain, as is generally the case in all industrialized countries, its incidence has increased over recent years. Furthermore, despite advances in its treatment, it represents 41% of all deaths due to digestive system cancers in the world. It is the second leading cause of death by cancer, exceeded by lung cancer in men and breast cancer in women, with an overall mortality rate of 40-50%.
Definición
Colon or rectal cancer is also known as colorectal cancer. Symptoms may include blood in the stool, thinner stools, changes in bowel habits and general stomach discomfort. If it is detected early, it is often curable.
Diagnóstico
The exact origin of colorectal cancer is still unknown, but there are multiple factors influencing this neoplastic process. These include:
- Genetic Factors: the appearance of colorectal cancer is possibly the result of a series of events starting with a chromosomal mutation or a similar process followed by progression phenomena in which both genetic and environmental factors may be involved.
- Inflammatory bowel disease: there is an increased risk of colon cancer (30 times higher) in patients with inflammatory bowel disease. However, of all the patients diagnosed with colorectal cancer, only 1% have a history of inflammatory bowel disease.
- Dietetic factors have also been linked to the etiology of colorectal cancer. Although studies conducted are not conclusive regarding the exact role of dietetic factors, it seems that diets high in fat and low in fiber play an important role in the development of colorectal cancer. The importance of fiber lies in its capacity to bind bile acids and various carcinogens in the intestinal lumen and its fecal flora-modifying and intestinal transit-accelerating effects, which reduces the intraluminal concentration of carcinogenic or co-carcinogenic substances and reduces contact time between carcinogenic or co-carcinogenic substances and the colonic mucosa.
- Pelvic radiotherapy has been associated with the development of colon neoplasia with a mean interval to onset of 15.2 years.
- Other more controversial factors include a sedentary lifestyle, the use of oral contraceptives, giving birth, morbid obesity and a high concentration of iron in feces.
Colorectal cancer is not just an isolated disease. It can also occur in the context of clinical syndromes such as adenomatous polyposis syndromes and hereditary non-polyposis colon cancer.
Intestinal polyposis syndromes can be classified as:
- Hereditary
- Adenomatous polyps
- Familial polyposis of the colon or familial adenomatous polyposis *LINK
- Gardner syndrome
- Turcot syndrome
- Hamartomatous polyps
- Juvenile polyposis syndrome
- Peutz-Jeghers syndrome
- Neurofibromatous polyposis
- Cowden syndrome
- Ruvalcaba-Myhre-Smith syndrome
- Devon polyposis syndrome
- Non-hereditary
- Cronkhite-Canada syndrome
- Hyperplastic polyposis
- Inflammatory polyposis
- Lymphoid nodular hyperplasia
- Lymphomatous polyposis
Tratamiento
The treatment of colon cancer is always surgical and the surgery performed must comply with a series of principles to guarantee curative resection, known as adequate oncological resection. The principles of curative resection for colorectal cancer include excision of the primary tumor with adequate proximal, distal and lateral margins for local and regional tumor control, ensuring a secure, well-vascularized and tension-free anastomosis. The extent of the resection is determined by the site of the tumor, its vascularization, its lymphatic drainage and the presence or absence of direct extension into adjacent organs, ensuring en bloc resection of the entire area infiltrated by neoplasia.
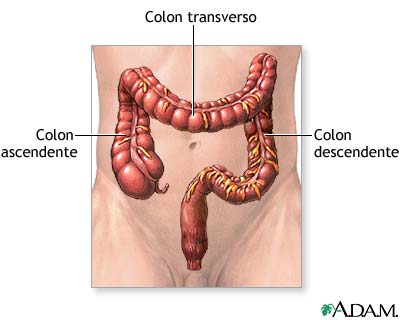
Figure 1. Colon anatomy
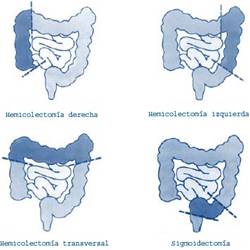
Types of surgery:
-
Laparoscopic surgery in colorectal cancer
Numerous papers analyzing the results of prospective series comparing laparoscopic and conventional surgery in the treatment of colorectal cancer have shown that laparoscopic resection in the treatment of neoplastic diseases can be performed just as safely as open surgery, guaranteeing oncological resection of the segment of colon to be removed including resection of the blood vessels and excision of the corresponding lymph nodes.
Studies published to date enable us to answer three questions about the application of laparoscopy in the treatment of colorectal cancer in favor of laparoscopic surgery:
- Are the short-term post-operative outcomes more favorable in patients undergoing operations for colon neoplasia using laparoscopic surgery techniques?
- Can laparoscopic surgery guarantee the same oncological resection and tumor staging as conventional surgery in patients with colon neoplasia?
- Does laparoscopic surgery affect the long-term survival of patients?
-
Right hemicolectomy
For tumors found in the cecum and ascending colon, the required surgery is a right hemicolectomy. The vascular section should include the ileal marginal arterial arcade, the ileocolic artery, the right colic artery and the right branch of the middle colic artery. The lymphatic territory should include the lymph nodes in the mesocolon and the lymph node chains from the ileocolic and right colic arteries to the edge of the superior mesenteric artery.
-
Extended right hemicolectomy
For tumors of the hepatic flexure and the proximal half of the transverse colon, an extended right hemicolectomy will be performed in which the middle colic artery should be ligated at its origin at the level of the tail of the pancreas.
-
Left hemicolectomy
For tumors of the splenic flexure, distal half of the transverse colon and descending colon, the surgery of choice is a left hemicolectomy with proximal ligation of the inferior mesenteric vessels and excision of the lymph nodes of the corresponding mesocolon and the main lymph node chains of the inferior mesenteric artery.
-
Sigmoidectomy
For tumors in the sigmoid colon, the standard surgery is a sigmoidectomy with ligation of the inferior mesenteric artery at its origin. The extent of the resection will depend on the segment of sigmoid colon affected. Lesions of the proximal sigmoid colon will require an anastomosis between the descending colon and the distal sigmoid colon, lesions of the distal sigmoid will require an anastomosis between the proximal sigmoid and the upper rectum and lesions of the middle sigmoid, depending on the redundancy of the sigmoid colon, will require an anastomosis between the sigmoid-descending colon and the rectosigmoid junction.
-
Subtotal colectomy
A subtotal colectomy is indicated in patients with synchronous carcinomas in different parts of the colon. Other indications for subtotal colectomy include: presence of multiple polyps not resected by endoscopy and young patients with a family history.
Figure 2. Types of colon resection